Medication of l-tetrahydropalmatine significantly ameliorates opiate craving and increases the abstinence rate in heroin users: a pilot study1
Introduction
Drug addiction, a chronic brain disease, is characterized by constant relapse that requires long-term treatment[1]. Currently, the first line of treatment for chronic opioid dependence is agonist maintenance treatment, such as methadone and buprenorphine. The principle of maintenance treatment is to suppress withdrawal symptoms and heroin craving, reducing heroin abuse and the risks associated with drug use behaviors[2,3]. Fundamentally, however, the maintenance treatment is not an abstinence-oriented program. Once the maintenance program is interrupted, the protracted abstinence withdrawal syndrome (PAWS) will occur, resulting in relapse.
New pharmacological strategies that target specific elements of the addiction cycle are currently under intense investigation. For example, naltrexone, an opioid receptor antagonist, was initially developed to treat heroin dependence by blocking euphoria and weakening the addiction cycle. In clinical practice, however, naltrexone produced adverse effects and did not ameliorate the PAWS of opiate dependence, resulting in a lower retention rate and relapse [4]. So far, pharmacological agents have shown limited efficacy in the treatment of drug addiction[5]. There are no broadly effective anti-relapse pharmacotherapies available for human opiate dependence.
The major problem in the clinical treatment of drug dependence is relapse. Many addicts respond very well to inpatient treatment and yet their relapse occurs soon after leaving the program. The addiction neurobiology, based on decades of animal studies, suggests that the onset of heroin withdrawal coupled with reward deficits could play a critical role in provoking craving and relapse in human opiate addicts[6]. We hypothesized that if a medication, without reinforcing abuse potential, could effectively ameliorate the PAWS of opiate dependence, especially the drug craving, the medication could be effective in reducing the relapse rate. To test this hypothesis, we employed rotundine, that is, l-tetrahydropalmatine (l-THP), in this pilot study.
l-THP is a main active ingredient of a Chinese traditional analgesic herb and has been safely prescribed in Chinese clinical settings for more than 40 years. l-THP significantly binds to dopamine (D1, D2, and D3) receptors[7–12] and antagonizes morphine abuse in animal experiments[13–15]. Recent reports showed D3 to be significantly involved in drug craving and relapse processes[16–18]. Further, l-THP has no abuse potential and its pharmacology and neuropsychopharmacology have been extensively studied with animals and human models. These results have been widely published, particularly in Chinese literature[19]. Finally, since l-THP is already listed in Chinese pharmacopeia, the associated costs and time required to conduct clinical trials would be substantially reduced.
We report our initial results in a randomized, placebo-controlled, and double-blinded study with l-THP treatment after 7–10 d of detoxification. We demonstrate that l-THP treatment significantly ameliorates the PAWS, especially drug craving, and increases abstinence rate among heroin users.
Materials and methods
l-THP l-THP is a purified compound isolated from Chinese herbs by Best & Wide Pharmaceutical (Nanning, China). It has been approved by the Chinese Government Agency since 1964 (State Food and Drug Administration of China), and listed in Pharmacopoeia of China (1977 edition) for human use in relief of chronic pain, insomnia, and anxiety.
Human patients In total, 120 heroin-dependent patients (27.57±5.76 years old, mean±SD, 89 males and 29 females) were recruited during the study period between June 2000 and February 2001 from the inpatient population at the Hengyang Detoxification Clinic (HDC), Hunan, China. Each participant met the DSM-IV criteria for heroin dependence and was tested as having a positive opiate in his or her urine test before entering the HDC. The patients expressed their willingness to participate in this trial. Exclusion criteria included any drug dependence other than tobacco and opiates; history of psychiatric and neurological diseases, such as schizophrenia, psychosis, past seizure episode, or current use of psychoactive medications; hepatic, cardiovascular, and renal diseases; and pregnancy or breastfeeding. Written informed consent was obtained from each patient, and the human protocol was approved by the IRB of Second Xiangya Hospital (Changsha, China).
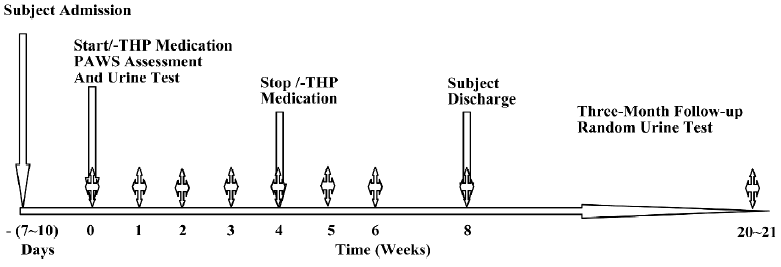
Study design A randomized, double-blinded, placebo-controlled trial was designed. As shown in Figure 1, participants had been detoxified in a ward at the HDC and were abstinent for at least 7 d before entering the trial. The participating patients remained in a ward during this trial. The participants were randomly divided into 2 groups: the l-THP treatment group (2 tablets [30 mg l-THP] twice per day) and the placebo group (2 placebo tablets twice per day). The treatment dose was selected based on the preclinical and clinical studies in order to minimize its mild sedative effects, which began to manifest at a higher dose (>100 mg/70 kg body weight). The l-THP and the placebo tablets were provided by Best & Wide Pharmaceutical (China). The l-THP medication lasted for 1 month, while participants stayed in the clinic as inpatients. After the cessation of l-THP treatment for 1 month, the participants either stayed in the clinic or decided to return home. Urine samples were collected to test for heroin or morphine by 8 different intervals: day of admission, d 7, 14, 21, and 28 during l-THP medication, and on d 5, 14, and 28 after the cessation of the medication. During the following 3 months after the patients were discharged, the random urine tests were conducted to check their abstinence-free status for the residual of heroin or morphine. During the 5 month study period, participants could discontinue the study at any time. No patient received psychotherapy. The PAWS severity was determined by completing a questionnaire at the 8 time intervals, as described earlier.
The questionnaire measuring the severity of the PAWS, termed the Heroin Withdrawal Scale (HWC), was specifically developed and validated for opiate dependence[20]. As listed in Table 2, this self-rating scale consists of 30 symptoms in 4 categories: 9 symptoms in the mood category, 8 symptoms in the craving category, 4 symptoms in the insomnia category, and 9 symptoms in the somatic category. The intensity of each symptom was rated with a 5 point scale of 0=not at all, 1=a little, 2=moderately, 3=quite a bit, and 4=extremely). The rated scores for each symptom in the same category from every patient were added up as the categorized score for the patient. The categorized scores from individual patients in a group were then averaged to obtain the mean±SD. The higher the scores were, the more severe the PAWS.
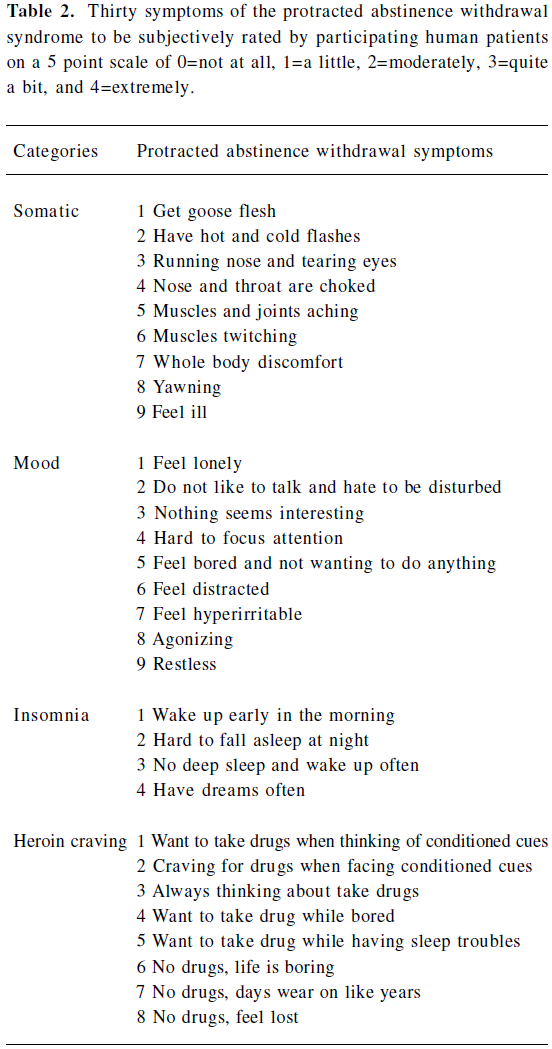
Full table
End-points of the study Retention in treatment and abstinence rates were employed as the end-points. No information was collected from patients who left the trial program. These patients were categorized as “relapsed” when determining the abstinence rate. Other outcome measures included changes in the PAWS severity scores (HWC-30) for mood, craving, sleep, and somatic symptoms. The higher the scores, the more severe the syndrome.
Data analysis The Kaplan–Meier method was employed to estimate the event-free survival probability of patient retention in the treatment program, and the log–rank test was used to analyze the retention rate between the l-THP-treated group and the placebo group. Considering the effects of antagonistic mechanisms of l-THP treatment on the mood syndrome, the estimations were conducted in 2 time periods: the first was done in the initial 2 weeks, and the other was accomplished during the rest of trial period. The differences in severity among the PAWS scores and the individual PAWS categorical ratings for “somatic”, “mood”, “sleeping”, and “craving” were analyzed with the following time-dependent regression model:
Yk,i,j=mk(ti,j)+εk,i,j, for k=1, 2; i=1, …, nk; j=1, 2, …, 8,
where tk,i,j= (0, 7, 14, 21, 28, 35, 42, and 56 d) are observation times, Yk,i,j is the jth measurement of the ith patient from the kth treatment group, and εk,i,j are the 0 mean error terms. The testing null and alternative hypotheses are:
H0: m1(tj)=m2(tj) for all j=1, 2, …, 8 versus HA: m1(tj) ≠ m2(tj) for some j.
The differences in the severity scores of the PAWS measurements between the treated and placebo groups were assessed using the method of comparing cross-section growth data[21,22]. This method compares the difference of the areas under the regression curves (ie it examines whether there is an overall difference between the 2 groups). When a significant difference is detected, the Student t-test method can be used to identify differences at a given time point.
Results
Demographics and clinical characteristics of participating patients Table 1 lists the demographics and clinical characteristics of the participants taken from the Selected Structured Clinical Interview for the DSM-IV diagnoses at intake. None of the variables differed in terms of sex, age, education, the kind of treatment, the age of onset, and the daily time of heroin administed between the l-THP-treated group and the placebo group. No significant differences were evident in these demographics between the 2 groups.
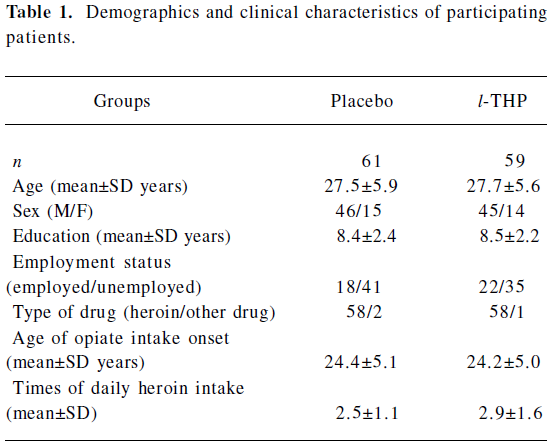
Full table
Comparison of the dropout rates and abstinence rates after l-THP medication The results of the retention for the l-THP-treated and placebo groups are shown in Figure 2 by the Kaplan–Meier estimators. After medication for 2 weeks, the survival probability of retention for the placebo group was 100% (95% confidence interval [CI]: 100%–100%), while that of the l-THP-treated group was 72% (95% CI: 60%–83%). The log–rank test showed that the dropout rate for the l-THP-group was significantly higher than that of the placebo group (Figure 2A; Table 3, P<0.0001). The placebo group retained 59 patients in the trial program, whereas the medication group decreased from 61 patients to 44 (Figure 2A; Table 3).
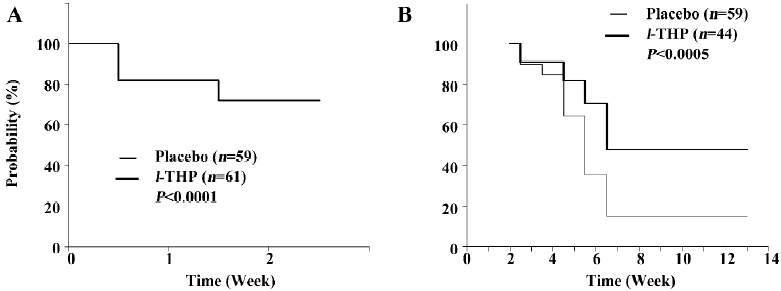
Full table
After the 3 month follow-up observation, it was noted that participants who survived the 2 weeks of medication and remained in the trial program had a high abstinence rate of 47.7% (95% CI: 33%–67%) as opposed to the placebo group of 15.2% (95% CI: 7%–25%). The log–rank test has a P-value of 0.0005, indicating that the abstinence rate was significantly higher in the treatment group than the placebo group (Figure 2B).
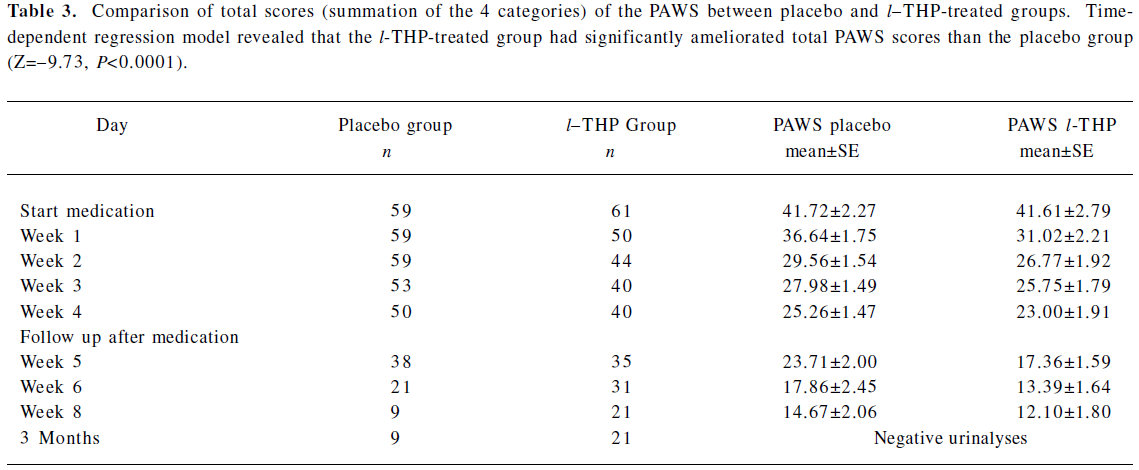
Effects of l-THP medication on total scores and the 4 categories of the PAWS According to the regression analysis, 1 month of l-THP medication significantly reduced the total scores of the PAWS severity, as shown in Table 3 (Z=-9.73; P<0.0001). The l-THP-treated group showed a significant reduction in severity than the placebo group in the somatic syndrome (Figure 3A; Z=-6.082; P<0.0001), insomnia (Figure 3C; Z=-6.399; P<0.0001), and craving (Figure 3D; Z=-22.42; P<0.0001), but not in the mood state (Figure 3B; Z=0.2568; P=0.7973).
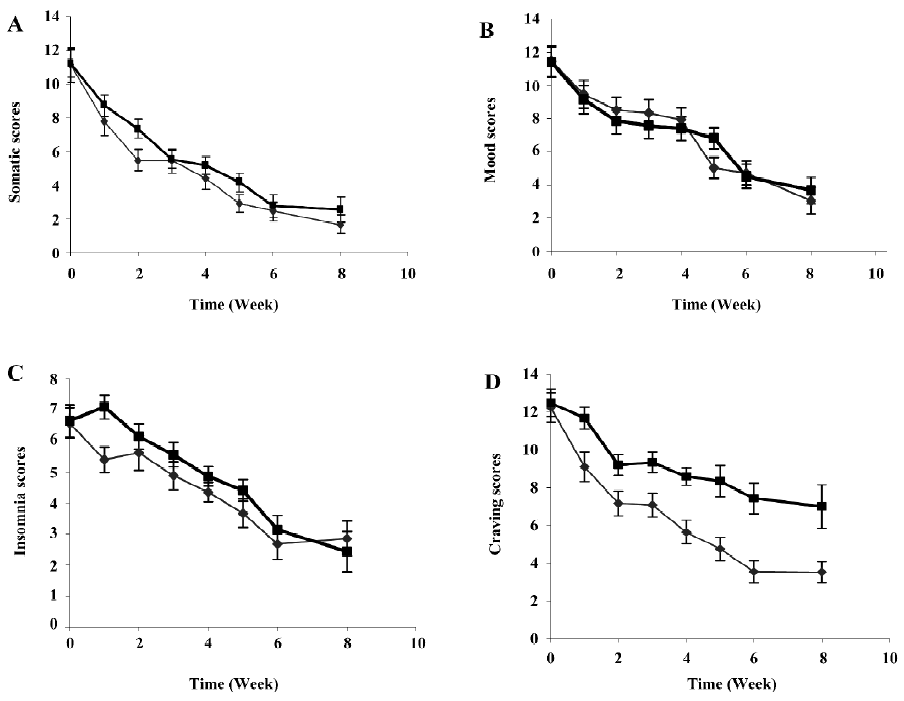
The most intriguing result of the l-THP treatment was the significant reduction in opiate craving (Figure 3D). After 1 week of treatment with l-THP, the craving scores were substantially reduced compared to the placebo group, and continued to decline thereafter. One month after the cessation of treatment, the craving score was 3.5±2.6 (mean±SD) for the treatment group versus 7.0±3.5 for the placebo group (P<0.01; Figure 3D).
Discussion
l-THP has an antirelapse effect The present study supported a clinical hypothesis that continued treatment is necessary beyond detoxification, even when the body is cleansed of the drug. Our experimental results demonstrated that l-THP medication can significantly reduce the severity of the PAWS, especially opiate craving, and increase the abstinence rate after medication. Our preliminary results demonstrated that proper medication, such as l-THP, could be effective in decreasing opiate relapse.
The present study design has a unique feature in that the administration of l-THP was given after 7–10 days of drug abstinence. Since the main goal of this study is to test if l-THP is effective as an antirelapse medication, it is necessary for patients to achieve a drug-free state first, at least for a period of time, then determine the relapse rate from the drug-free state. There was difficulty in ascertaining the ideal length of the drug-free state. It is noteworthy that in the Kaplan–Meier curves in Figure 2A, the retention rate was significantly lower after 2 weeks of l-THP treatment, as opposed to the placebo group. The treatment retention rate was improved after 14 d of l-THP medication, as shown in Figure 2B. It is denoted that a period of drug-free state requires at least a 2 week trial period of l-THP. The detailed mechanisms underlying the lower retention rate in the first 2 weeks are not clear. Among these unscheduled early termination cases, there were no reports of adverse effects or acute hepatic toxicity due to the l-THP treatment. The effects of the dopaminergic antagonisms of l-THP could have played a role in early discharge. A previous study suggested that chronic heroin users might produce a reduction in dopaminergic activity in the human brain[18]. The antagonisms of l-THP medication could reduce the post-synaptic dopaminergic activities further, resulting in lower retention. After the 2 weeks, the dopaminergic activities may recover and the retention rate may be improved significantly. This mechanism may be similar to that evidenced in clinical practice whereby naltrexone treatment may not be given to heroin users until they have a negative reaction to naloxone. However, in animal studies, l-THP could enhance the presynaptic dopaminergic activity, including biosynthesis and release of dopamine via the feedback regulation[38-40]. This mechanism might be involved in the early termination cases.
Alternatively, we suggest that in the morphine users, the brain function of endogenic opioid peptides, such as endophine (μ agonist) and enkephalin (δ agonist), have not dropped away from the substitutive inhibition of morphine (an exogenic μ and δ agonist) during the 10 d period. Under these in vivo circumstances in the brain, the D2 antagonism of l-THP would aggravate the substitutive inhibition of heroine users. The above-mentioned animal results[38-40] would support this idea. However, in the animal experiments, the D2 antagonism of l-THP was substantiated to be an augmentation on the brain function of endophrine in the periaqueductal gray (PAG), and enkphrine in the brain[19,31,32,41]. Since the main goal of this study was to test if l-THP is effective as an anti-relapse medication, it is necessary that patients achieve a long drug-free state first, followed by l-THP treatment to prolong heroin abstinence. Based on this observation, it is suggested that patients be tested 21–30 d before l-THP medication, rather than the current 7-10 d. This should allow a higher retention rate during the early treatment period.
Possible mechanism of l-THP treatment for heroin abstinence First, l-THP is an antagonist of DA receptors[7-11]. Its antagonistic effect on DA receptors, particularly D2 and D3 receptors, would play an important role in reducing drug craving. Many recent studies using animal models have demonstrated that l-THP is a potential candidate for treating heroin[12-15] and cocaine addiction[23-25]. Other studies have shown that D3 receptor antagonism significantly inhibits cocaine-seeking behavior[26-28] and reduces nicotine-paired environmental cue functions[29].
The D2 receptor, like DA (D2 and D3) receptors, display a presumed pharmacological similarity and homology in the sequence of amino acids, which increased up to 75% in the 7 transmembrane domains. It has been shown that D3 receptors are mainly located post-synaptically, and a subset of D3 receptors is located presynaptically. The neuroanatomical locations of D3 receptors are mainly restricted to expression in distinct areas of the limbic system, such as the nucleus accumbens and the islands of Calleja. The nucleus accumbens is involved in the diverse neurological and psychiatric disorders, such as Parkinson’s disease, schizophrenia, and drug abuse (heroin, morphine, cocaine etc), which have been extensively reviewed[16,30].
Second, it has been shown that the antinociception of l-THP is based on the antagonism on the D2 and D3 DA receptors in the ventral tegmental area (VTA)–accumbens nucleus–prefrontal cortex DA pathway[19], and the D2 receptors in the arcuate nucleus of the hypothalamus is also involved in l-THP-induced, β-endorphin neuron-mediated analgesic action[19,31], which projects to PAG, an important action site of morphine. It has been observed that l-THP acts on the arcuate nucleus and has a sequential enhancement of END release, which modulates the physiological functions, such as analgesia or anticraving resulting from long-time exposure to morphine[32,33]. As well as this, D2 and D3 antagonism of l-THP would interrupt the DA transporter function in the nucleus accumbens on the pre- and post-synaptic sites[11,34,35].
Furthermore, brain DA neurons in heroin addicts may become maladapted due to long-term exposure to morphine and could be readapted by l-THP treatment. In the experiment of morphine-dependent rats, the levels of glial fibrillary acidic protein (GFAP) and tyrosine hydroxylase (TH) in the DA neurons of the VTA were significantly increased. l-THP treatment significantly decreased the levels of GFAP and TH in the VTA to normal levels, indicating that the function of the dopaminergic neurons is in recovery[36]. Similarly, l-THP treatment can reverse the decreases of dopamine D1 and D2 receptor mRNA in morphine-dependent rats[37]. These results suggest that l-THP treatment can facilitate the recovery of dopaminergic functions and gene expression.
Recent studies have demonstrated that l-THP treatment could produce a rightward and downward shift in the dose–response curve for cocaine self-administration and attenuate cocaine-induced reinstatement[23,24]. It is presumed that the cocaine-induced DA transporter-mediated effect is reduced by the D2 and D3 antagonism of l-THP on the post-synaptic site in the nucleus accumbens, which may be potentially of use in treating human cocaine addiction.
Limitations of this pilot study This pilot study demonstrated that l-THP significantly ameliorated the PAWS, especially reducing drug craving and increasing the abstinence rate among heroin users. These results support the potential use of l-THP for the treatment of heroin addiction. However, there are several methodological limitations to be addressed. First, the study participants were mixed between treatment seekers and non-treatment seekers, since they were recruited from the compulsory detox institution. It is possible that treatment seekers and non-treatment seekers may have different responses to l-THP treatment. Second, the present study employed only pharmacotherapy with l-THP medication without cognitive behavioral treatment (CBT). It is expected that the combination of CBT with pharmacotherapy may produce a synergistic effect. Third, the present study has been limited to employing only 1 dose of l-THP with a short duration (1 month). Although the short duration and the low dose of l-THP were initially chosen to reduce the risk of possible hepatic toxicity[42], a future study may examine the effects of the length of treatment time, number of treatment sessions, and dose responses.
Acknowledgements
We thank Dr Gao-hong WU and Mr Douglas WARD for statistical analysis, and Ms Carrie O’CONNOR for editorial assistance.
References
- O’Brien CP. Anticraving medications for relapse prevention: a possible new class of psychoactive medications. Am J Psychiatr 2005;162:1423-31.
- Haasen C, van den Brink W. Innovations in agonist maintenance treatment of opioid-dependent patients. Curr Opin Psychiatr 2006;19:631-6.
- Sung S, Conry JM. Role of buprenorphine in the management of heroin addiction. Ann Pharmacother 2006;40:501-5.
- Dackis C, O’Brien C. Neurobiology of addiction: treatment and public policy ramifications. Nat Neurosci 2005;8:1431-6.
- Heidbreder CA, Hagan JJ. Novel pharmacotherapeutic approaches for the treatment of drug addiction and craving. Curr Opin Pharmacol 2005;5:107-18.
- Kenny PJ, Chen SA, Kitamura O, Markou A, Koob GF. Conditioned withdrawal drives heroin consumption and decreases reward sensitivity. J Neurosci 2006;26:5894-900.
- Xu SX, Yu LP, Han YR, Chen Y, Jin GZ. Effects of tetrahydrop-rotoberberines on dopamine receptor subtypes in brain. Acta Pharmacol Sin 1989;10:104-10.
- Jin GZ. (–)-Tetrahydropalmatine and its analogues as new dopamine receptor antagonists. Trends Pharmacol Sci 1987;8:81-2.
- Jin GZ, Wang XL, Shi WX. Tetrahydroprotoberberine – a new chemical type of antagonist of dopamine receptors. Sci Sin [B] 1986;29:527-34.
- Jin GZ, Xu SX, Yu LP. Different effects of enantiomers of tetrahydropalmatine on dopaminergic system. Sci Sin [B] 1986;29:1054-64.
- He Y. The pharmacological properties of -stepholidine on different dopamine receptor subtypes [PhD Dissertation]. Shanghai: Shanghai Institute of Materia Medica, 2005.
- Hong Z, Fan G, Le J, Chai Y, Yin X, Wu Y. Brain pharmacokinetics and tissue distribution of tetrahydropalmatin enantiomers in rats after oral administration of the recemate. Biopharm Drug Dispos 2006;27:111-7.
- Wang YB, Ren YH, Zheng JW, Zeng I. Influence of l-tetrahydropalmatine on morphine-induced conditioned place preference. Chin Pharmacol Bull 2005;21:1442-5.
- Wang YB, Ren YH, Zheng JW. The effects of l-THP on morphine-induced discrimination. Chin J Drug Dependence 2005;14:27-9.
- Liu YL, Liang JH, Yan LD, Su RB, Wu CF, Gong ZH. Effect of l-tetrahydropalmatine on locomotor sensitization to oxycodone in mice. Acta Pharmacol Sin 2005;26:533-8.
- Heidbreder CA, Gardner EL, Xi ZX, Thanos PK, Mugnaini M, Hagan JJ, et al. The role of central dopamine D3 receptors in drug addiction: a review of pharmacological evidence. Brain Res Rev 2005;49:77-105.
- Pilla M, Perachon S, Sautel F, Garrido F, Mann A, Wermuth CG, et al. Selective inhibition of cocaine-seeking behaviour by a partial dopamine D-3 receptor agonist. Nature 1999;400:371-5.
- Kish SJ, Kalasinsky KS, Derkach P, Schmunk GA, Guttman M, Ang L, et al. Striatal dopaminergic and serotonergic markers in human heroin users. Neuropsychopharmacology 2001;24:561-7.
- Jin GZ. Discoveries in the voyage of corydalis research. Shanghai: Shanghai Scientific & Technical Publishers; 2001.
- Chen HX, Hao W, Yang DS. The development of subjective protracted withdrawal scales for opiate dependence. Chin J Mental Health 2003;17:294-7.
- Scheike TH, Zhang MJ. Cumulative regression function tests for regression models for longitudinal data. Ann Statistics 1999;26:1328-55.
- Scheike TH, Zhang MJ, Juul A. Comparing reference charts. Biometrical J 1999;41:679-787.
- Luo JS, Ren YH, Zhu R. The effect of l-THP on cocaine-induced conditioned position preference. Chin J Drug Depend 2003;12:177-9.
- Mantsch JR, Li SJ, Risinger R, Awad S, Katz E, Baker DA, et al. Levo-tetrahydropalmatine attenuates cocaine self-administration and cocaine-induced reinstatement in rats. Psychopharmacology 2007;192:581-91.
- Xi ZX, Yang Z, Li SS, Li X, Dillon C, Pang XQ, et al. Levo-tetrahydropalmatine inhibits cocaine’s rewarding effects: Experiments with self administration and brain-stimulation reward in rats. Neuropharmacology 2007;53:771-82.
- Vorel SR, Ashby CR Jr, Paul M, Liu X, Hayes R, Hagan JJ, et al. Dopamine D3 receptor antagonism inhibits cocaine-seeking and cocaine-enhanced brain reward in rats. J Neurosci 2002;22:9595-603.
- Xi ZX, Gilbert J, Campos AC, Kline N, Ashby CR Jr, Hagan JJ, et al. Blockade of mesolimbic dopamine D3 receptors inhibits stress-induced reinstatement of cocaine-seeking in rats Psychopharmacology (Berlin) 2004;176:57-65.
- Xi ZX, Newman AH, Gilbert JG, Pak AC, Peng XQ, Ashby CR Jr, et al. The novel dopamine D3 receptor antagonist NGB 2904 inhibits cocaine’s rewarding effects and cocaine-induced reinstatement of drug-seeking behavior in rats. Neuropsychopharmacology 2006;31:1393-405.
- Pak AC, Ashby CR Jr, Heidbreder CA, Pilla M, Gilbert J, Xi ZX, et al. The selective dopamine D3 receptor antagonist SB-277011A reduces nicotine-enhanced brain reward and nicotine-paired environmental cue functions. Int J Neuropsychopharmacol 2006;9:585-602.
- Joyce JN, Millan MJ. Dopamine D3 receptor antagonists as therapeutic agonists. Drug Dis Today 2005;10:917-25.
- Hu JY, Jin GZ. Supraspinal D2 receptor involved in antinociception induced by l-tetrahydropalmatine. Acta Pharmacol Sin 1999;20:715-9.
- Hu JY, Jin GZ. Arcuate nucleus of hypothalamus involved in analgesic action of l-THP. Acta Pharmacol Sin 2000;21:439-44.
- Ge XQ, Lin AP, Sun Y, Zhou HZ, Zhang HQ, et al. Effects of l-tetrahydropalmatine on opioid peptides contents in morphine dependent rats. Chin Pharmacol Bull 2001;17:264-6.
- Liu YL, Liang JH, Yan LD, Su RB, Wu CF, Gong ZH. Effects of l-tetrahydropalmatine on locomotor sensitization to oxycodone in mice. Acta Pharmacol Sin 2005;26:533-8.
- Wang W, Zhou Y, Sun J, Pan L, Kang L, Dai Z, et al. The effect of l-stepholidine, a novel extract of Chinese herb, on the acquisition, expression, maintenance, and re-acquisition of morphine conditioned place preference in rats. Neuropharmacology 2007;52:356-61.
- Yang Z, Li CO, Fan M. Effect of tetrahydroprotoberberines on contents of glial fibrillary acidic protein and tyrosine hydroxylase in ventral tegmental area of morphine dependent rats. Chin J Pharmacol Toxicol 2003;17:246-50.
- Yang Z, Li CQ, Fan M. Effects of tetrahydroprotoberberines on expression of dopamine system related genes in morphine dependent rats. Chin J Psychiatr 2004;37:111-5.
- Marcenac F, Jin GZ, Gonon F. Effect of l-tetrahydropalmative on dopamine release and metabolism in the ret striatums. Psychopharmcology 1986;89:89-93.
- Huang KX, Sun BC, Gonon F, Jin GZ. Effects of tetrahydroproto-berberines on dopamine release and 3,4-dihydroxyphenylacetio acid level in corpus striatums measured by in vivo voltammetry. Acta Pharmacol Sin 1991;12:32-6.
- Chen LJ, Guo X., Wang QM, Jin GZ. Feed-back regulation of presynaptic D2 receptors blockaded by l-stepholidine and l-tetrahydropalmatine. Acta Pharmacol Sin 1992;13:442-5.
- Hu JY, Jin GZ. Effect of tetrahydropalmatine analogs on Fos expression. Acta Pharmacol Sin 1999;20:193-200.
- Lai CK, Chan A YW. Tetrahydropalmatine poisoning: diagnoses of nine adult overdoses based on toxicology screens by HPLC with diode-array detection and Gas chromatography-mass spectrometry. Clin Chem 1999;45:229-36.
